Previous issue | Next issue | Archive
![]() Volume 11 (5); September 25, 2021 [Booklet]
Volume 11 (5); September 25, 2021 [Booklet]
Dexmedetomidine for sedation and correction of psychoemotional disorders in critically ill patients with COVID-19
| Dexmedetomidine for sedation and correction of psychoemotional disorders in critically ill patients with COVID-19 |
Ibadov RA, Arifjanov ASh, Ibragimov SKh, and Khakimov BB.
J. Life Sci. Biomed., 11(5): 80-87, 2021; pii:S225199392100010-11
DOI: https://dx.doi.org/10.51145/jlsb.2021.10
Abstract
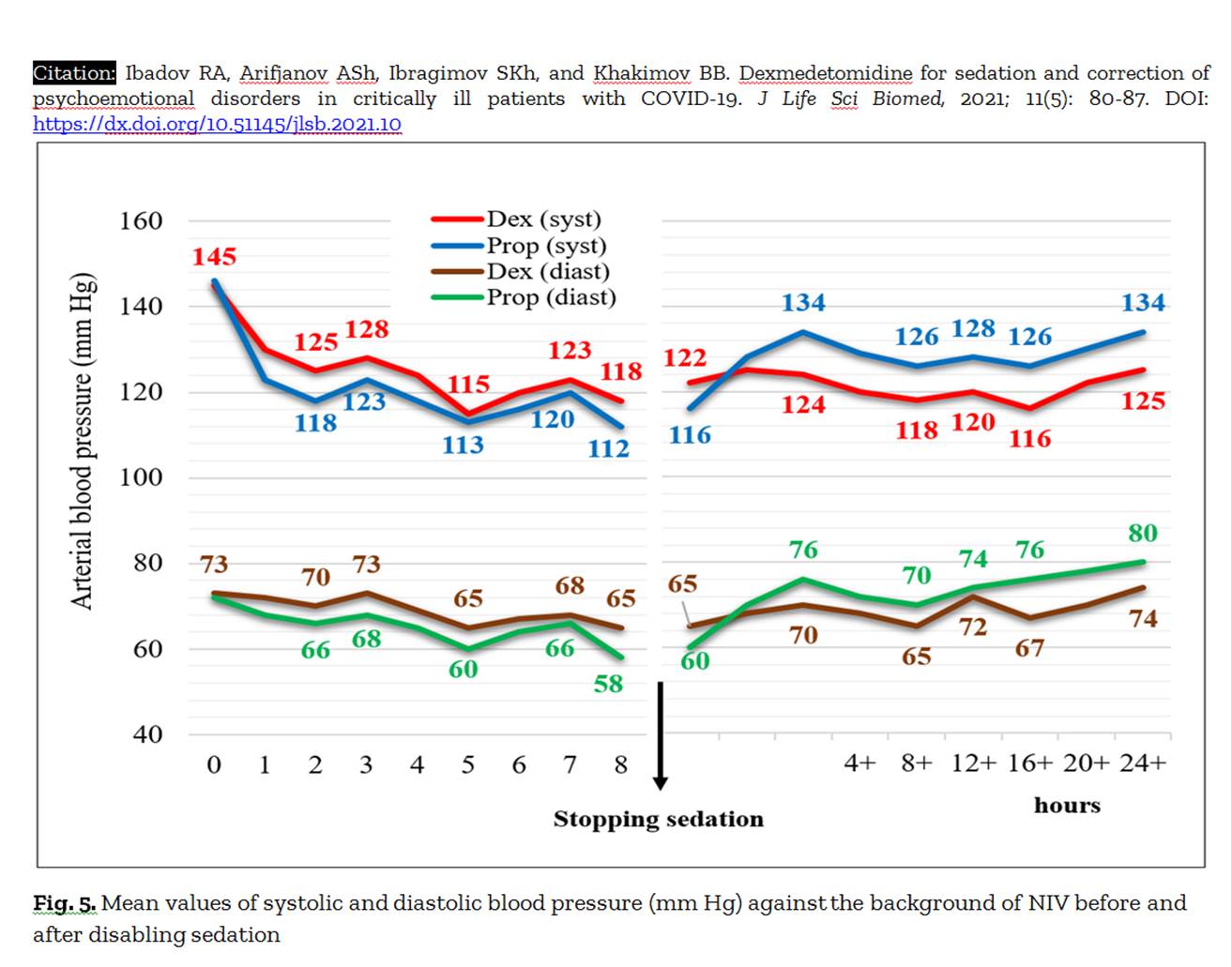
Aim. The objective of this study was to evaluate sedation therapy effectiveness in critically ill patients with severe COVID-19 who received dexmedetomidine compared to propofol. Methods. The research was done in a prospective single center to a cohort study of critically ill 333 adult patients with COVID-19 and psychoemotional disorders (depression, anxiety and posttraumatic stress disorder) admitted in the ICU of the Republican Specialized Hospital for COVID-19 in Uzbekistan. Patients were non-invasive ventilated more than 24 hours and received intravenous sedation with dexmedetomidine or propofol. Results. The risk of progression of the pathological process decreased from 47.6% to 21.8% and, accordingly, the proportion of patients with stabilization and improvement of their condition increased from 52.4% to 79.4% (p<0.001). The possibilities of non-invasive respiratory support were expanded with a reduction in the frequency of tracheal intubations from 17.3% to 7.3% (p<0.001), the duration of ICU stay was from 12.6±0.8 to 9.4±0.6 days, and the duration of respiratory therapy was from 8.4±0.5 to 5.2±0.4 days. In particular, there was an improvement in oxygen saturation (SpO2) recovery after one day of intensive therapy from 86.6±0.2% to 92.2±0.3% with non-invasive ventilation and a higher oxygenation index (2.3 in the dexmedetomidine group versus 1.6 in the propofol group, p=0.032) during the period of sedation withdrawal. Conclusion. In the presence of severe psychoemotional disorders, the effectiveness of etiotropic and pathogenetic treatment protocols of COVID-19 directly depends on the proper sedation regimen. In this aspect, dexmedetomidine provides adequate and safe respiratory support with an improvement in external respiration, blood gas composition and a minimal negative hemodynamic effect.
Keywords: COVID-19, Intensive care unit, Depression, Anxiety, Posttraumatic stress Disorder, Sedation, Dexmedetomidine, Comparison study
[Full text-PDF] [XML] [PubMed-XML] [ePub] [Export citation to BibTeX, RIS & EndNote] [How to Cite] [Semantic Scholar]
Efficacy of multisensory exercise programme on cognition and functionality in postmenopausal women
| Efficacy of multisensory exercise programme on cognition and functionality in postmenopausal women |
Abd El-Hay RA, Hanafy HM, Kamel HE, and Mahmoud AM.
J. Life Sci. Biomed., 11(5): 88-93, 2021; pii:S225199392100011-11
DOI: https://dx.doi.org/10.51145/jlsb.2021.11
Abstract
Introduction. In the last century, longer female life expectancy has implied that women now live a third of their lives beyond the end of their ovarian function, increasing the need for new therapeutic strategies to facilitate successful aging (defined as low probability of disease), high cognitive and physical abilities, and active engagement in life. Aim. This study was conducted to determine the efficacy of multisensory exercise programme on cognition and functionality in postmenopausal women. Methods. Thirty postmenopausal women in the range of 55-65 years old and a body mass index (BMI) < 35kg/m² were selected randomly from physiotherapy outpatient clinic at Al-Menshawy General Hospital. They were randomly distributed into two equal groups: control group (A) that received relaxation training programme for 30 minutes/session, three sessions per week for a period of 4 weeks and study group (B) which received multisensory exercise programme for another 45 minutes per session plus the same programme as for control group for a period 4 weeks. Assessment of all women in both groups was carried out before and after treatment programme (four weeks) through cognitive assessment (montreal cognitive assessment) and functional performance of daily living activities (nine–item physical performance test). Results. The multisensory exercise programme showed statistically significant improvements (P < 0.01) on cognition, and functional performance as compared with the control group, which showed no statistically significant differences at the post intervention time point. Conclusions. The multisensory exercise programme improved the cognition and functionality of post menopausal women. The introduction of a motor and multisensory‐based approach in care routines may improve residents' health and engagement to the environment.
Keywords: Aging, Cognition, Multisensory exercise, Menopause, Residential care homes.
[Full text-PDF] [XML] [ePub] [PubMed-XML] [Export citation to BibTeX, RIS & EndNote] [How to Cite] [Semantic Scholar]